The human brain can change – but usually only slowly and with great effort, such as when learning a new sport or foreign language, or recovering from a stroke. Learning new skills correlates with changes in the brain, as evidenced by neuroscience research with animals and functional brain scans in people. Presumably, if you master Calculus 1, something is now different in your brain. Furthermore, motor neurons in the brain expand and contract depending on how often they are exercised – a neuronal reflection of “use it or lose it.”
People may wish their brains could change faster – not just when learning new skills, but also when overcoming problems like anxiety, depression and addictions.
Clinicians and scientists know there are times the brain can make rapid, enduring changes. Most often, these occur in the context of traumatic experiences, leaving an indelible imprint on the brain.
But positive experiences, which alter one’s life for the better, can occur equally as fast. Think of a spiritual awakening, a near-death experience or a feeling of awe in nature.
Social scientists call events like these psychologically transformative experiences or pivotal mental states. For the rest of us, they’re forks in the road. Presumably, these positive experiences quickly change some “wiring” in the brain.
How do these rapid, positive transformations happen? It seems the brain has a way to facilitate accelerated change. And here’s where it gets really interesting: Psychedelic-assisted psychotherapy appears to tap into this natural neural mechanism.
Psychedelic-assisted psychotherapy
Those who’ve had a psychedelic experience usually describe it as a mental journey that’s impossible to put into words. However, it can be conceptualized as an altered state of consciousness with distortions of perception, modified sense of self and rapidly changing emotions. Presumably there is a relaxation of the higher brain control, which allows deeper brain thoughts and feelings to emerge into conscious awareness.
Psychedelic-assisted psychotherapy combines the psychology of talk therapy with the power of a psychedelic experience. Researchers have described cases in which subjects report profound, personally transformative experiences after one six-hour session with the psychedelic substance psilocybin, taken in conjunction with psychotherapy. For example, patients distressed about advancing cancer have quickly experienced relief and an unexpected acceptance of the approaching end. How does this happen?
Research suggests that new skills, memories and attitudes are encoded in the brain by new connections between neurons – sort of like branches of trees growing toward each other. Neuroscientists even call the pattern of growth arborization.
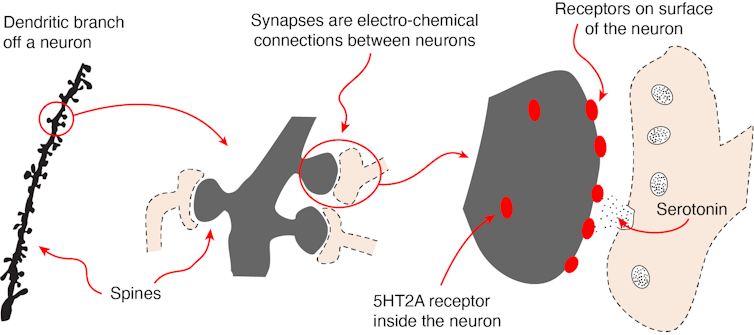
Researchers using a technique called two-photon microscopy can observe this process in living cells by following the formation and regression of spines on the neurons. The spines are one half of the synapses that allow for communication between one neuron and another.
Scientists have thought that enduring spine formation could be established only with focused, repetitive mental energy. However, a lab at Yale recently documented rapid spine formation in the frontal cortex of mice after one dose of psilocybin. Researchers found that mice given the mushroom-derived drug had about a 10% increase in spine formation. These changes had occurred when examined one day after treatment and endured for over a month.
A mechanism for psychedelic-induced change
Psychoactive molecules primarily change brain function through the receptors on the neural cells. The serotonin receptor 5HT, the one famously tweaked by antidepressants, comes in a variety of subtypes. Psychedelics such as DMT, the active chemical in the plant-based psychedelic ayahuasca, stimulate a receptor cell type, called 5-HT2A. This receptor also appears to mediate the hyperplastic states when a brain is changing quickly.
These 5-HT2A receptors that DMT activates are not only on the neuron cell surface but also inside the neuron. It’s only the 5-HT2A receptor inside the cell that facilitates rapid change in neuronal structure. Serotonin can’t get through the cell membrane, which is why people don’t hallucinate when taking antidepressants like Prozac or Zoloft. The psychedelics, on the other hand, slip through the cell’s exterior and tweak the 5-HT2A receptor, stimulating dendritic growth and increased spine formation.
Here’s where this story all comes together. In addition to being the active ingredient in ayahuasca, DMT is an endogenous molecule synthesized naturally in mammalian brains. As such, human neurons are capable of producing their own “psychedelic” molecule, although likely in tiny quantities. It’s possible the brain uses its own endogenous DMT as a tool for change – as when forming dendritic spines on neurons – to encode pivotal mental states. And it’s possible psychedelic-assisted psychotherapy uses this naturally occurring neural mechanism to facilitate healing.
A word of caution
In her essay collection “These Precious Days,” author Ann Patchett describes taking mushrooms with a friend who was struggling with pancreatic cancer. The friend had a mystical experience and came away feeling deeper connections to her family and friends. Patchett, on the other hand, said she spent eight hours “hacking up snakes in some pitch-black cauldron of lava at the center of the Earth.” It felt like death to her.
Psychedelics are powerful, and none of the classic psychedelic drugs, such as LSD, are approved yet for treatment. The U.S. Food and Drug Administration in 2019 did approve ketamine, in conjunction with an antidepressant, to treat depression in adults. Psychedelic-assisted psychotherapy with MDMA (often called ecstasy or molly) for PTSD and psilocybin for depression are in Phase 3 trials.![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.